#1 Endodontist Near Me
 Endodontics focuses on treating the inside of the tooth when it gets infected or damaged. The inside of the tooth is also known as the “pulp”. The most well known endodontic treatment that people are aware of is called a “root canal”. This is when the dentist goes in and removes infected pulp that is causing severe pain or other detrimental oral health issues. This procedure’s main goal is to relieve the patient from pain as well clean out the affected and dead tissues. On top of relieving you from pain, this allows you to keep as much of your natural tooth as possible.
Endodontics focuses on treating the inside of the tooth when it gets infected or damaged. The inside of the tooth is also known as the “pulp”. The most well known endodontic treatment that people are aware of is called a “root canal”. This is when the dentist goes in and removes infected pulp that is causing severe pain or other detrimental oral health issues. This procedure’s main goal is to relieve the patient from pain as well clean out the affected and dead tissues. On top of relieving you from pain, this allows you to keep as much of your natural tooth as possible.
Endodontic treatments can include many more procedures that just root canals. Treatments can include micro-surgical procedures that are just on the tips of a tooth’s root, treating dental trauma, and getting to the source of unexplained pain or discomfort. The field of endodontics offers many different ways of preserving a patient’s teeth and avoiding unsightly extractions or costly tooth-replacement options.
Tooth Pulp – The Inside of The Tooth
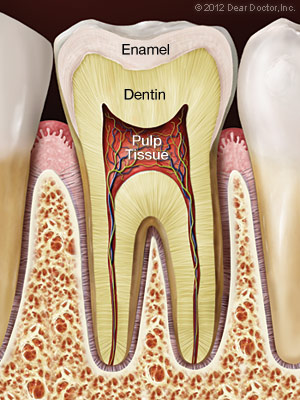
On the inside of each tooth is a “pulp” like material that is known as dentin. Dentin is actually what makes up the majority of the structure of your teeth. It also helps to form the root of the tooth as well. Dentin is also what sends nerve signals throughout your teeth. This is why teeth are capable of feeling multiple sensations.
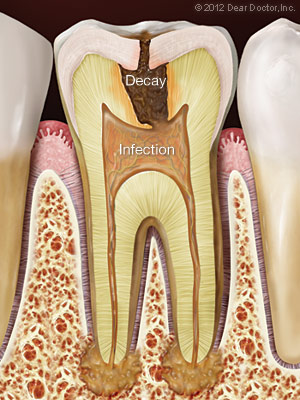
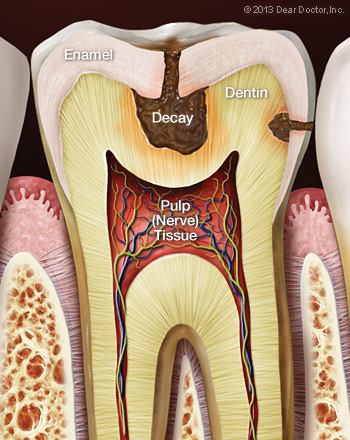
The soft tissue that is located beneath the crown, under the enamel, and deep within the root canals of the tooth is called the “pulp”. This area is where your tooth’s nerves and blood vessels can be found. When your teeth become victims of infection and become inflamed, the first sign is usually pain and discomfort. As time goes on and the nerve cells die, this pain and discomfort can often go away. The main issue still remains, though. When left untreated, infection deep within the pulp and roots can lead to tooth loss or even more damaging results.
Getting To The Root Of The Problem Dental Pain
Infections deep within the tooth are often what call for root canal treatment and the removal of the infected soft tissues. When tooth decay is left un-treated, this decay spreads. Not only does it go to other parts of the mouth, but also deeper within the tooth’s structure. If one of your teeth has been cracked or chipped, this leaves bacteria room to come in and infect the underlying structure and tissues of the tooth.
Treating Dental Trauma
A very common type of dental trauma are sports injuries. These account for the vast majority of dental injuries according to the American Dental Association. These injuries can very easily damage the tooth’s underlying structure, including the pulp or dentin. Be sure to always wear a mouthguard while playing sports to prevent any of these types of dental injuries. Sports injuries can, again, cause severe trauma to the teeth, which can require costly treatments to fix.
The Endodontic Treatment Process
People generally have a bad perception of root canals. The thing is that root canal treatments are performed to relieve pain rather than cause it. Most patients report feeling little to no pain or discomfort during a root canal treatment, and the procedure is very similar to getting a filling done.
Here are some of the things you can expect during a root canal treatment:
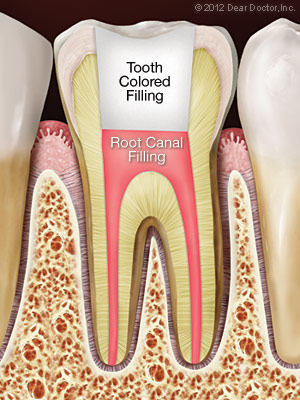
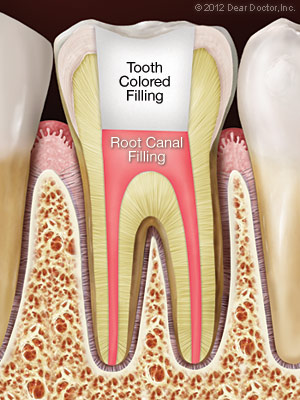
To start, your dentist will use local anesthetics around the area of the infected tooth and tooth root. For the vast majority of patients, the most painful and annoying part of the root canal procedure is now over! Then, the pulp of the tooth is accessed by an opening in the tooth and any dead tissue is removed using extremely precise tools and dental instruments. The individual root canals that are are affected are fully cleaned, disinfected, and any bacteria is then removed. Lastly, the tooth has a core buildup or is filled with a temporary filling until a crown can be placed on the tooth.
Your dentist may recommend other treatments if infection deep within one or multiple teeth is necessary. Sometimes, a crown or other restorative procedure may be necessary following your endodontic treatment in order to restore the appearance of your teeth. Whatever the case may be, know that with proper oral hygiene, the treatment you have received from your endodontist can last for the rest of your life!
 WHEN IS TOOTH EXTRACTION NECESSARY?
WHEN IS TOOTH EXTRACTION NECESSARY?
There are many different circumstances under which you might need to have you tooth extracted. Tooth decay may call for an extraction if it’s severe and causing damage to the underlying bone structure. Your dentist will be able to tell if an extraction is necessary, or if the tooth can be saved. If your tooth is tooth damaged to receive an endodontic treatments then an extraction may be necessary.
Depending on which treatments and procedures are necessary, your dentist will determine the best plan of action. Give us a call today to see if you need an endodontic treatments or an extraction!
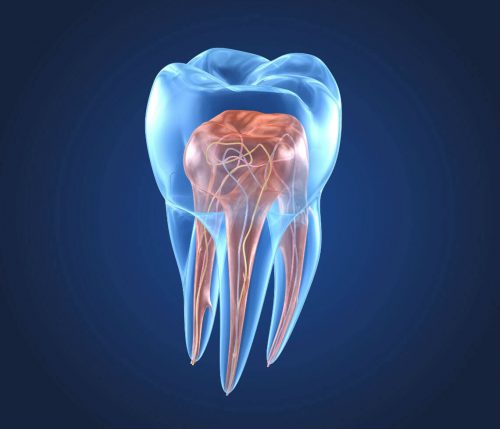
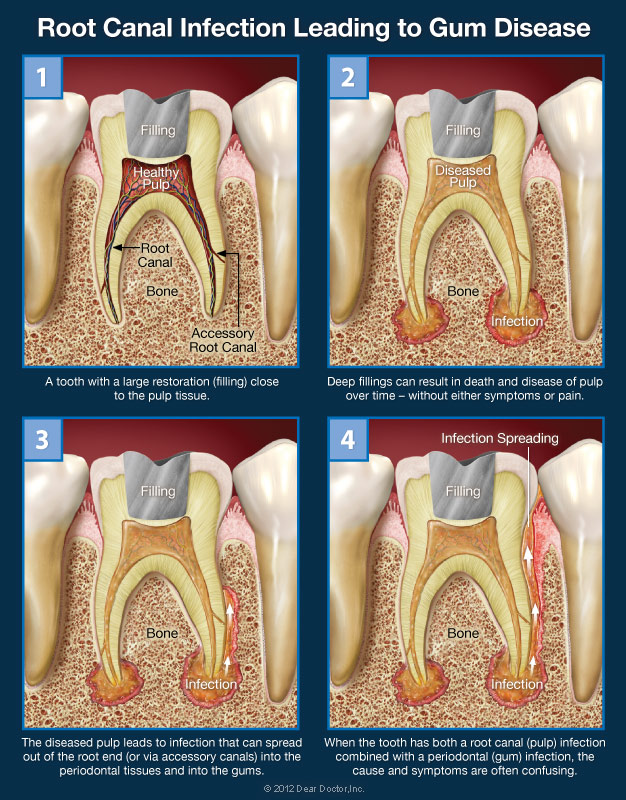
 Sometimes, getting to the source of tooth pain can be a difficult task. There are other times that it is clear where the pain is coming from. If you have more than one oral health issue, the pain can be harder to narrow down or require more treatment. One example of when this might happen is when there is infection in the tooth as well as the surrounding gum areas.
Sometimes, getting to the source of tooth pain can be a difficult task. There are other times that it is clear where the pain is coming from. If you have more than one oral health issue, the pain can be harder to narrow down or require more treatment. One example of when this might happen is when there is infection in the tooth as well as the surrounding gum areas.
When this is the case, decay often starts in the dentin and pulp of the tooth, and then spreads to the surrounding gum tissues. Your dentist will always perform an in-depth evaluation and exam of your teeth, gums and mouth in general to determine where the infection is and how it can be effectively treated as to not spread any further.
Not All Symptoms Mean The Same Thing
Tooth and gum pain can be occasional and intermittent. Other times it can be chronic and never let up. Sudden, intense pains can be caused by cold or hot food and drinks or even trauma and injury. There are times that the pain feels like pressure that is coming from an entire group of teeth, or other parts of the face and mouth, such as the sinus cavities.
Pinpointing the cause of these symptoms isn’t always the easiest task and can mean the pain could be coming from multiple areas. However, it should be noted that avoiding or dismissing these symptoms is never a good idea. What starts out as mild pain can turn into more severe symptoms if left untreated. Mild pain can go away if left untreated, but you should still visit a dentist. Mainly because this can mean that the nerves within the tooth have died, and need to be removed.
Not All Tooth Decay Symptoms Are Alike…
Root canal infections can spread to other parts of the mouth through cracks or openings in the tooth. This can then infect the gums or underlying bone structure. This can result in gum disease as well as other infections. When this occurs, severe pain can be the result, which lets you know which tooth exactly is infected.
The opposite is also true. Meaning that an infection that begins in the gums can also spread within the teeth and infect the pulp of the tooth. The infection enters the tooth through canals that are located around the root of the tooth. If you’ve recently chipped or cracked a tooth, this makes infection an even more likely possibility.
Treating Tooth Decay and Discomfort
When infection is present in both the teeth and surrounding gum tissue, treating the infection in its entirety can be tricky at times. Pinpointing where the infection began can be a challenge, as there are many different possibilities as to where it began. For instance, if the infection began within the gums, the infection began in the gum tissue and moved its way into the pulp of the teeth. However, if the infection began in the roots of the teeth, this means that the infection spread the other way around.
Whichever circumstance is present, your dentist will need to identify the source of your pain and then make a diagnosis and formulate a proper treatment plan. This is why it’s vital to see your dentist right as these symptoms are present. The sooner you get an exam, the better your chances are of saving your teeth and keeping a healthy smile!
Your teeth are remarkably strong, anchored in your jaw, and are covered by enamel. Even with them being as strong and sturdy as they are, it is still possible for them to chip, crack, or even break. There has actually been evidence that today, our teeth are developing cracks at record rates. This may be due to the fact that people are living longer, that our stress levels are increasing, and our diet has changed significantly.
Biting on hard foods and objects, being hit in the mouth, having large cavities, or old amalgam fillings can weaken the tooth’s structure. These are some common causes of tooth fractures. But, no matter the cause, there are a number of symptoms that indicate a tooth may be cracked. There are several treatments that we can provide depending on the severity of the injury.
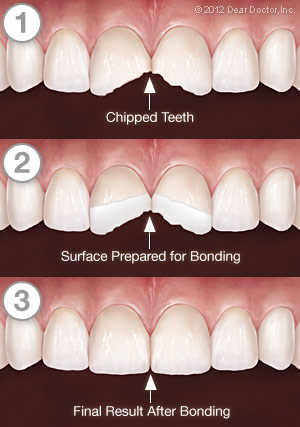
Small chips on the edges or cusps of teeth often cause no symptoms and can very easily be treated by cosmetic bonding or other methods. Deeply fractured and cracked teeth, on the other hand, may become a serious problem. The sooner they are treated, the more likely it is that the affected tooth can be saved. Let’s take a look closer look at the types of fractures teeth can develop, and the symptoms they may produce.
Minor Cracks (craze lines)
These tiny fissures in the outer enamel of the tooth often cause few to no symptoms at all. In fact, most require no treatment. If you are having tooth pain, however, these cracks will need to be evaluated and possibly treated. That’s because without a careful and proper examination, there is no way to know for sure whether these cracks only go in to the enamel, or if they penetrate into the dentin of the tooth. While the tiniest craze lines might not show up on X-rays, they can often be detected by feel, by having you close down on a “bite stick,” or by using special dye stains or high-magnification instruments.
 Vertical Cracks
Vertical Cracks
This type of crack often starts at the chewing surface and extends down toward the roots. Either way, it doesn’t completely separate the tooth into two parts. Depending on the extent of the fracture, you may feel only minor discomfort that occurs in response to temperature changes)or, when you chew. You definitely shouldn’t ignore these symptoms, because cracked teeth require dental treatment quickly to keep them from decaying or becoming infected. If the cracks continue to worsen, tooth extraction may become necessary.
Deep Fractures or Split Teeth
When serious fractures occur, you’ll know it! Large parts of the tooth can be separated from each other, and tooth’s pulp is often inflamed and painful. This condition requires immediate treatment, and it might not be possible to save the tooth.
Treatment for Cracked Teeth
What treatment is best for a cracked tooth depends on the extent and the severity of the damage. If a small crack is detected early enough, it is possible to use restorative materials to seal it. For larger cracks that can delve in to the pulp of the tooth, root canal treatment might be required. If a root canal is done, a crown will be placed to finish your restoration. Sometimes, additional procedures may be recommended to try and save the tooth. In the most severe cases you tooth might need to be extracted.
The most effective and preferred treatment for cracked teeth is prevention! Regular dental checkups, where your teeth are examined carefully for early signs of a problem can help with prevention as well. However, if you experience any symptoms that could indicate a cracked or broken tooth, please don’t wait. The sooner it’s treated, the better the chance that we can save it. Call us today if you need to schedule an appointment!
 Root canal therapy is an effective treatment at relieving tooth pain and halting infection of the soft tissues deep inside the teeth and gums. But occasionally the body may not heal as expected. After a period of time, you may experience pain in the affected tooth again, or even if you have no symptoms, x-rays may reveal that infection is still present near the tooth’s roots. In that case, you may need root canal re-treatment.
Root canal therapy is an effective treatment at relieving tooth pain and halting infection of the soft tissues deep inside the teeth and gums. But occasionally the body may not heal as expected. After a period of time, you may experience pain in the affected tooth again, or even if you have no symptoms, x-rays may reveal that infection is still present near the tooth’s roots. In that case, you may need root canal re-treatment.
There are several reasons why your root canal treatment may not have succeeded at first. The “canals” themselves are slender, forking passageways that are deep in your tooth that contain the nerves and blood vessels. The canals can be very narrow and some infection might still be present. Or, the canals might even have become recontaminated via a variation of ways like a delayed or ineffective crown restoration, new tooth decay, advancing gum disease, or even a cracked or fractured tooth. Any of these conditions could result in reinfection.
If initial root canal therapy has failed, the first thing to do is evaluate your options. Besides retreatment, the alternatives may include endodontic surgery or extraction of the affected tooth. A missing tooth, alternatively, should be replaced by a dental implant, a bridge or a partial denture as soon as possible. None of these are simple or inexpensive options. That’s the main reason that we prefer you keep your natural teeth whenever possible.
The Retreatment Procedure
If endodontic retreatment is a part of your treatment plan after you get reevaluated, do not stress out. The procedure is similar to your original root canal treatment and will not be painful. After you receive a local anesthetic, any restorations already on your tooth will be moved to provide access to the root canal filling material. This is usually accomplished by making a small opening into the inner part of the tooth, removing filling material or obstructions, and then cleaning the canals with precise tools.
A microscope and light are used to search carefully for additional canals or unusual structures that might cause problems in the future. If the treatment process becomes extremely complex, it may be followed up and finished in a subsequent visit. Finally, when all of the canals have been cleaned and disinfected, they will be filled with the proper filling materials and sealed. Then a temporary filling will be placed in or on the tooth. A permanent restoration will need to be placed and fitted at a later appointment.
Is Root Canal Retreatment My Best Option?
Modern medicine and dentistry are as much art as science, and neither one can guarantee that any procedure will be 100% successful. While endodontic retreatment can be more complex than initial root canal therapy, it offers a very solid chance of success in most cases. And, since the field of endodontics is constantly changing and becoming more modern, it is possible there are new techniques that weren’t available when your first root canal procedure was done.
Dentists take our responsibility seriously to help you understand the risks, benefits, and alternatives for treating root canal issues. When we recommend retreatment, it is because we feel it is the best way for you to preserve your natural teeth. And our goal is to have you enjoy your natural teeth for many years to come.
 Occasionally, root canal treatment can be unsuccessful at resolving an infection in the tissues near a tooth’s roots. That’s when a minor surgical procedure called an apicoectomy may be recommended. Because this procedure is often performed with the aid of a microscope and other precise and specialized tools, it is considered a type of “endodontic microsurgery”. This is probably the most common type of root canal surgery. An apicoectomy involves removing a small portion of the apex, or tip, of the tooth’s root along with any surrounding hard or soft tissue that may be infected.
Occasionally, root canal treatment can be unsuccessful at resolving an infection in the tissues near a tooth’s roots. That’s when a minor surgical procedure called an apicoectomy may be recommended. Because this procedure is often performed with the aid of a microscope and other precise and specialized tools, it is considered a type of “endodontic microsurgery”. This is probably the most common type of root canal surgery. An apicoectomy involves removing a small portion of the apex, or tip, of the tooth’s root along with any surrounding hard or soft tissue that may be infected.
What would cause you to need an apicoectomy? There could be several reasons, including a canal that can’t be accessed, an anatomical irregularity, or a fracture or crack in the tooth’s roots. The procedure is normally only recommended after one or more root canal treatments and retreatments has been attempted and failed. Since this type of problem generally occurs near the tip of the root, the procedure is a very effective way to treat a persistent infection.
Before an apicoectomy procedure, X-rays of the affected tooth and surrounding bone, a careful review of your medical history including medications you take, and other factors are reviewed. If an apicoectomy is recommended, the reasons and options for it will be explained to you.
The Apicoectomy Procedure
Root canal surgery is usually performed under local anesthesia in the form of a numbing shot, so you won’t feel any pain. To begin the procedure, a small incision is made in the gum, and the infection that is at the end of the tooth’s roots is exposed. The infected tissue is then removed along with a few millimeters of the root tip itself. A dye may be used to help make cracks or fractures easy to see if there are any. If we discover that the tooth is fractured, it may be better to extract it at this time instead of completing the procedure.
Next, a microscope and light are used to examine the canals. They will be cleaned up, then filled with an inert material and sealed up with a small filling. To finish the procedure, a small bone graft may be placed at the affected site. Then the gum tissue covering the tooth’s root will be sewn closed. X-rays may be taken once more as the procedure nears completion. Afterwards, instructions on postoperative care will be given. Most apicoectomies take between 30 to 90 minutes to complete.
Following the procedure, you may experience some swelling and soreness in the area that was treated. Over-the-counter anti-inflammatory medications are usually all that’ is needed to mitigate any pain or discomfort. You can return to normal activities the following day, but you may want to avoid eating hard or crunchy foods or brushing vigorously for a few days afterwards. If your sutures aren’t self-dissolving, you will be asked to return in about a week to have them removed.
The Goal: Saving Your Tooth
Although apicoectomy is typically a safe and effective procedure, there are slight risks with any type of minor surgery. That’s why apicoectomies are not recommended unless further root canal treatment or retreatment won’t be an effective procedure. An alternative treatment in most cases would be an extraction of the tooth. However, our goal as dentists is to help you preserve your natural teeth for as long as possible.
While there are excellent and effective methods of tooth replacement such as dental implants, these involve further and more complex treatments or surgery. On top of that they can be costly procedures. An apicoectomy is generally a permanent and cost-effective solution which can help the tooth last for the rest of your life!
 Root canal treatment and endodontics is a set of specialized procedures designed specifically to treat problems of the soft pulp tissue inside your tooth. While some mistakenly think of it as an unusually painful treatment, for most people the procedure is no more uncomfortable than getting a filling. It is one of the most effective ways of relieving tooth pain and preserving natural teeth.
Root canal treatment and endodontics is a set of specialized procedures designed specifically to treat problems of the soft pulp tissue inside your tooth. While some mistakenly think of it as an unusually painful treatment, for most people the procedure is no more uncomfortable than getting a filling. It is one of the most effective ways of relieving tooth pain and preserving natural teeth.
A root canal procedure becomes necessary when infection or inflammation develops in the soft tissue and pulp area of the tooth. Pulp tissue consists of blood vessels, connective tissue, and nerve cells, all of which explains why an infection or injury can cause severe pain. In time, the pain may go away at least temporarily. Without treatment, however, the infection won’t and it can lead to a dental abscess or may even contribute to systemic problems in other parts of the body.
Root Canal Treatment Is Virtually Painless
Most people have the perception that a root canal is the worst dental treatment around. The art of dentistry has become so advanced that this is no longer true by any means. The idea that a root canal procedure comes with severe pain and problems is a myth. But, it is certainly true that infection or inflammation in the tooth’s pulp can be excruciatingly painful. You should remember that having a root canal results in eliminating this acute pain and is not the cause of the pain.
Need another reason not to delay root canal treatment? A natural tooth that’s saved via root canal treatment and restoration helps you avoid the problems that can occur when teeth must be removed. This can include unwanted tooth migration or shifting, which can lead to difficulties in chewing. You might even end up needing treatment for bridgework or dental implants, which may be costly and complicated. An extraction can even lead to the eventual loss of bone structure from the area of the missing tooth.
 Causes of Root Canal Problems
Causes of Root Canal Problems
Root canal problems stem from infection and inflammation of the tooth’s pulp tissue. One potential cause of infection is deep tooth decay. Untreated dental cavities eventually allow bacteria to work their way down to the center of the tooth, where they may infect the pulp tissue. Another path by which bacteria may come into contact with pulp is via chipped, cracked, or damaged teeth. Any opening in the protective enamel coating has the potential to allow bacteria access to the tooth’s pulp.
In some cases, extensive dental work itself may cause damage to the pulp tissue that will need to be treated via root canal. Having multiple fillings or restorations on the same tooth increases the chances of this type of issue to occur. Occasionally, common procedures like crown preparation or orthodontics may eventually lead to root canal problems.
 What to Expect During Root Canal Therapy
What to Expect During Root Canal Therapy
If an examination shows that you do need root canal therapy, you don’t need to worry. It is one of the most routine and effective procedures that dentists can perform and can often be accomplished in just one visit.
The root canal process generally begins the same way as a filling does, and with no greater discomfort. A local anesthetic is administered to numb the tooth and the surrounding areas. For a lot of patients, the worst is already over.
Next, a small opening is made in the surface of the affected tooth to give the dentist access to the pulp chamber and root canals. Precise instruments are used to remove the dead and dying pulp from inside these narrow canal passageways. The chamber and empty canals are then cleaned, disinfected, and prepared to receive a filling of inert material. Finally, adhesive cement is used to seal the opening in the tooth, preventing any future infection.
Following root canal treatment, your tooth may feel some sensitivity, pain, or tenderness for a few days. Over-the-counter pain relievers like ibuprofen are generally effective in relieving discomfort and inflammation. But, prescription medications may also be given if needed. During this period, it may help to avoid biting hard on the affected tooth. All of these symptoms should be temporary.
To further protect the tooth and restore it to full function, it is usually necessary to have a crown or other type of restoration placed on it. Restorations can take many forms, from traditional silver crowns, to gold crowns, and in most cases porcelain. In any case, you will have made an investment in preserving your dental health and natural teeth for years to come.
Signs and Symptoms of Root Canal Problems
How do you know when you need a root canal? Sometimes, it is painfully obvious. If you feel constant and severe pain and pressure in your mouth, or noticeable swelling and extreme sensitivity in your gums, then it’s clear you need to make an appointment at our office and get treatment immediately. Another telltale symptom of pulp damage is sharp pain when you bite down on food. Lingering pain after eating hot or cold foods cam also be an indication of trouble. If you notice any of these symptoms, please call our office right away with one of our amazing dentists.
 If you have been told you need root canal treatment, you may be feeling a bit nervous. There is no need to stress because treating root canal problems is a routine treatment in modern dentistry that can relieve certain kinds of tooth pain and help your teeth last much longer. As you learn more about this beneficial procedure, you will understand why it’s needed and how it will leave your oral health in better shape and leaving you feeling better than before. Here are some answers to frequently asked questions:
If you have been told you need root canal treatment, you may be feeling a bit nervous. There is no need to stress because treating root canal problems is a routine treatment in modern dentistry that can relieve certain kinds of tooth pain and help your teeth last much longer. As you learn more about this beneficial procedure, you will understand why it’s needed and how it will leave your oral health in better shape and leaving you feeling better than before. Here are some answers to frequently asked questions:
What is a root canal?
Dentists use the term “root canal” in referring to the narrow passageways that branch from the pulp chamber down to the ends of the tooth roots. The term can also be used as a shorthand for “root canal treatment”. That is the procedure used to save the tooth if the soft tissue deep inside of it becomes inflamed or severely infected.
Why do I need root canal treatment?
If tooth pulp becomes infected and you are experiencing pain due to decay or injury, the soft tissue within the tooth will need to be removed in order to save the it and stop the infection from spreading. As an adult, you don’t actually need the pulp because its primary use is to aid in tooth development during childhood.
Is there an alternative?
You could have the whole tooth extracted, but it’s always better to try to save it. especially since root canal treatment is routine and has a very high success rate (over 90%). Saving the tooth can prevent other troubles from occurring later on. Some of those issued could include bite problems from teeth shifting position, difficulty eating, and loss of jawbone volume and density.
Is root canal treatment painful?
The procedure normally causes no more discomfort that a filling would. Root canal treatment may have a bad reputation, but it is undeserved. In other words, the infections that make the treatment necessary in the first place is often the painful part of the procedure because it is inflaming the tissue that has lots of nerves and is very sensitive. Root canal treatment actually relieves this pain!
What will happen during the procedure?
After numbing the area, a tiny hole in the top of your tooth is made to access the pulp chamber and canals. The infected tissue is removed, and the pulp chamber and the canal(s) are disinfected all the way to the ends of the root. Teeth in the front of the mouth have one root and generally one canal, while back teeth have two or three roots and generally three or four canals. Those canals and the pulp chamber are filled with an inert material and then sealed with adhesive cement. The access hole will receive a temporary filling.
What will happen afterwards?
Your tooth may feel sensitive for a few days, but any discomfort can usually be relieved with over-the-counter pain medication or anti-inflammatories. You will be instructed to avoid chewing on that tooth until it receives its permanent filling or crown, which can, and will, be placed a few days later. Depending on how damaged the tooth was to begin with will depend on the restoration and crown you receive. Those options will be discussed with you during your visit.
How can I avoid the need for root canal treatment in the future?
Keep your teeth decay-free and healthy by brushing and flossing every single day. Eat a healthy diet low in fats and sugars and be sure to avoid acidic beverages such as soda. Have regular professional cleanings and exams on top of at home hygiene. And, if you’re active in sports, consider getting a custom-made mouthguard to protect your teeth from injury.
 Root canal treatment is a safe and effective way to stop many kinds of tooth pain and to keep a tooth from being lost due to severe decay or injury. But, if a root canal is recommended for your child, you may be wondering why. Isn’t that baby tooth going to fall out in a few years anyway?
Root canal treatment is a safe and effective way to stop many kinds of tooth pain and to keep a tooth from being lost due to severe decay or injury. But, if a root canal is recommended for your child, you may be wondering why. Isn’t that baby tooth going to fall out in a few years anyway?
That’s true, the primary teeth typically are out between the ages of 6 and 12 years. Yet, there are some beneficial reasons for trying to save baby teeth for as long as possible with root canal treatment, rather than simply extracting any that are damaged by trauma or infection.
For one, primary teeth have the same functions as adult teeth and a missing tooth at any age can cause problems with speech, eating, and eventual tooth growth. Baby teeth also have another important role. They serve as guides for the proper placement of the permanent teeth. Without primary teeth to guide them in, permanent teeth tend to emerge crooked and often become tilted or crowded because of inadequate space. This can result in bite problems that may require extensive and expensive orthodontic treatment later on in life.
 Saving The Tooth Is Always Best
Saving The Tooth Is Always Best
Unlike its hard outer surface, the soft pulp inside the tooth is rich in blood vessels and nerves. Problems in this area are often signaled by tooth sensitivity and pain. When these symptoms occur, x-rays are often necessary to confirm that the pulp is diseased, or even dying. That is typically when treatment is needed, before an abscess or further infection can develop.
In severe cases, the tooth may need to be removed, and a space maintainer installed to fill the gap. But many times, space maintainers don’t fully restore the tooth’s functionality. Plus, the spacers are susceptible to coming loose and must be monitored constantly. If possible, other treatment methods are preferred, such as:
- Indirect pulp treatment. If pulp damage is minimal, it’s possible to remove most of the decay but not the pulp, apply an antibiotic, and then seal the tooth up again. This is referred to as an “indirect” treatment.
- Pulpotomy. Alternatively, if decay is limited to the upper portion of the pulp, we may recommend a “pulpotomy.” This involves removing the damaged part of the pulp, stabilizing the remaining healthy portion, and then disinfecting and sealing the tooth. This “partial” root canal is a time-tested technique that’s successful in a multitude of cases.
- Pulpectomy. If pulp tissue is infected through the entire tooth structure, a pulpectomy may be needed. This requires the removal of all pulp tissue. The canals are then disinfected, shaped, then filled and sealed with inert material. Afterwards, the crown of the tooth will be restored. This resembles traditional root canal therapy, with a crucial difference. That being the sealant we use in children is capable of being dissolved by the body. That way, when it’s time for a permanent tooth to erupt, the baby tooth’s roots can be naturally absorbed and tooth development can proceed normally.
Preparing for Your Child’s Root Canal Treatment
As you probably already know, most of the legends you may have heard about root canal therapy simply aren’t true. In fact, the procedure generally causes little discomfort, and is rather successful in relieving tooth pain! Dentists are very adept at using anesthesia to block any pain, and are experienced in calming the fears of young ones. While it’s understandable that you may be nervous, it will help if you don’t let your child pick up on your own anxiety. A calming voice and a gentle touch can do a lot to relieve their stress.
After a thorough examination, the best options for your child’s treatment will be recommended and a treatment plan will be created. These procedures are routine and follow-up instructions will be provided. A root canal is nothing you or your child should be afraid of. Think of it as a treatment that may save your child from some tooth pain now, and potentially a lot of corrective dental work later on in life.
 If your teeth seem especially sensitive after you brush them or when you consume certain foods or beverages, you are not alone. By one estimate, around 35 percent of the U.S. population experiences some degree of tooth sensitivity. While the difference between sensitivity and pain can become somewhat blurry, we can say that sensitive teeth usually produce discomfort in response to temperature swings, pressure, or even the sweetness of particular foods. What causes tooth sensitivity and what should you do about it?
If your teeth seem especially sensitive after you brush them or when you consume certain foods or beverages, you are not alone. By one estimate, around 35 percent of the U.S. population experiences some degree of tooth sensitivity. While the difference between sensitivity and pain can become somewhat blurry, we can say that sensitive teeth usually produce discomfort in response to temperature swings, pressure, or even the sweetness of particular foods. What causes tooth sensitivity and what should you do about it?
In general, tooth sensitivity results when dentin, the living tissue that makes up most of the “body” of the tooth, begins transmitting sensations to nerves deep in the tooth’s inner core. The nerves relay these sensations to the brain, and they’re felt as pain. To understand how this works, let’s take an even closer look at your teeth.
Tooth Anatomy 101
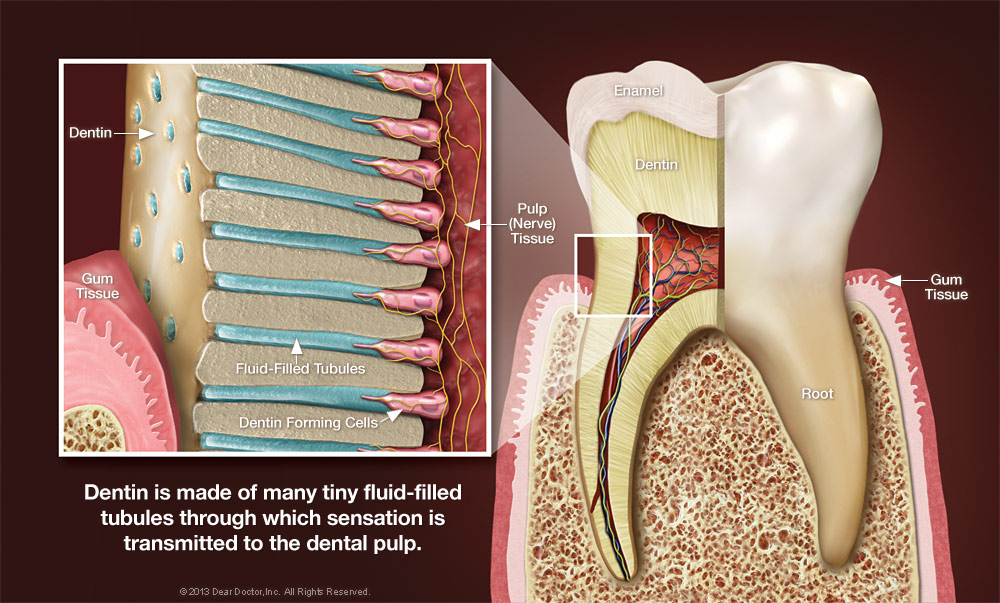
Dentin is a sturdy, calcified tissue, that can’t usually be seen. It’s normally covered by super-hard enamel on the crown of the tooth, and by softer tissue called cementum on the tooth’s roots, which typically lie below the gum line. The dentin itself is composed of many tiny tubules. When these tubules become exposed to the environment of the mouth, tooth sensitivity and pain may become persistent.
There are several reasons why the dentin can become exposed. For one, the gums may recede and shrink, which reveals some of the tooth’s root surfaces. This can be caused by genetic factors, periodontal disease, excessively vigorous brushing, or a combination of all three. This problem may be worsened if the tooth’s roots weren’t completely covered by cementum during their development, as sometimes occurs.
Another factor that may contribute to sensitivity is the erosion of tooth surfaces due to excessive acid in an individuals diet. While acids occur naturally in the mouth and certain foods, habitually drinking sodas and sports drinks can severely erode teeth And consequently, brushing soon after you drink actually worsens the effect. That’s because these acids soften the outer surfaces of the teeth, and brushing them makes it easy to wear them away. It’s best to wait for an hour afterwards, to give your saliva a chance to neutralize the acid.
Tooth decay can also cause sensitivity. Decay may not only expose dentin, but can work its way down to the nerves themselves. At that point, your pain level may increase dramatically. Sometimes, even dental work itself can cause sensitivity. Because the same tooth structures are involved, it may sometimes take a few days after a cavity is filled, for example, for a tooth to “calm down” and feel normal.
 Dealing With Tooth Sensitivity
Dealing With Tooth Sensitivity
What can you do about sensitive teeth? If it’s a relatively minor irritation, try not to brush the affected teeth too long or hard. Make sure you’re using a soft-bristled brush and the proper, gentle brushing technique. Always use a toothpaste containing fluoride. This ingredient is proven to increase the strength of tooth enamel, which helps resist erosion and decay. You can also try a toothpaste with ingredients designed specifically for sensitive teeth, such as potassium. Studies show that these can be effective but it may take time, approximately 4 – 6 weeks, for you to notice the difference.
If sensitivity persists, however, or if your tooth pain becomes more intense, don’t wait around to get an examination to determine what’s causing the problem. Once diagnosed, the most appropriate way to reduce the sensitivity will be recommended and given to you in your treatment plan. Some treatments may include concentrated fluoride varnishes, prescription mouthrinses, or bonding that is place on the outer surfaces of teeth. But tooth sensitivity may also be an early warning sign of other dental problems and the sooner you get to a dentist, the sooner it gets taken care of!
 Teeth whitening is one of the most popular cosmetic dental treatments and it is extremely easy to see why. Having whiter teeth can make you look years younger, and the procedure itself is among the most conservative and cost effective cosmetic treatments modern dentistry can offer. Sometimes, achieving a pleasing and even shade of white can be challenging. This is particularly true when a tooth that needs to be whitened has been the subject of an injury in the past.
Teeth whitening is one of the most popular cosmetic dental treatments and it is extremely easy to see why. Having whiter teeth can make you look years younger, and the procedure itself is among the most conservative and cost effective cosmetic treatments modern dentistry can offer. Sometimes, achieving a pleasing and even shade of white can be challenging. This is particularly true when a tooth that needs to be whitened has been the subject of an injury in the past.
Dental trauma encompasses any damage to the tooth that’s caused by an external force, whether accidental or intended. It may be due to a fall, a sports injury, car accident, or even a past orthodontic procedure. According to some studies, around a quarter of Americans aged 6 to 50 years old have experienced some traumatic dental injury, with most occurring before the age of 19. Traumatized teeth may react to whitening procedures differently from undamaged teeth, which can make them difficult to whiten. However, several effective treatments are available.
Diagnosing a Discolored Tooth
The first step in the process of whitening a traumatized tooth is a thorough examination to find out what’s causing the dark spots or staining. One of the first things we will determine is whether or not the tooth’s pulp is “vital,” or alive. This is readily revealed by x-rays or other tests. If the tooth is still vital, external bleaching can often yield amazing results, even if it’s just one of your teeth that needs to be whitened. In-office treatments or take-home trays are effective, but office procedures generally take much less time to produce great results.
Discoloration of a traumatized tooth is itself an indication that the nerves in the tooth’s pulp have died. In this case, before whitening treatment can start, a root canal procedure will be necessary to remove the decayed tissue and prevent infection. Even after a root canal has been performed, a tooth can become discolored over time. In either situation, it may be possible to whiten a non-vital tooth with a procedure called internal bleaching.
 Whitening From the Inside Out
Whitening From the Inside Out
Because a non-vital tooth’s stains are inside, rather than outside of the tooth, we need to put the bleaching agent itself in to the tooth. Internal bleaching is a routine procedure, here’s how it works:
Access to the pulp chamber will be gained by making a small hole in the back of the tooth. Then, any debris from the chamber will be removed and rinsed away, and a special cement will be added to prevent the bleaching agent from leaking into the tooth’s vital roots.
Next, some bleaching agent (commonly sodium perborate) will be placed in the empty pulp chamber, and temporarily seal it in. At this point, you can get up and leave the office, which is why this procedure sometimes is called the “walking bleach” technique. However, you will have to return in a few days for another round of bleaching. It is possible that it can take up to four visits to get the degree of whitening you are desiring.
When the tooth reaches the desired color you are looking for, a permanent restoration will be placed on the tooth to seal the hole used to put the bleach in. It is usually a tooth-colored filling material made out of composite resin. Many times, this relatively conservative procedure will give your tooth all the whitening that it needs. If it’s not enough, the tooth can be bleached externally as well! Or, you can even consider a veneer or crown for a different cosmetic treatment. The goal is to recommend the most appropriate cosmetic dental procedure, and get you the best possible results. Call our office today to get the best whitening procedures around!
MOST INSURANCES WELCOME AND MAXIMIZED!
NEW PATIENT SPECIALS & FINANCING OPTIONS AVAILABLE.
Contact us and schedule your visit today.
The Proof is in Our Patients
Contact Us For a Consultation
Open Daily For Your Convenience!
Monday 8:30 am – 5:00 pm
Tuesday 8:30 am – 5:00 pm
Wednesday 8:30 am – 5:00 pm
Thursday 8:30 am – 5:00 pm
Friday 8:30 am – 3:00 pm
OUR LOCATION
Spring Klein Endodontics
| Monday | 8:30 AM – 5:00 PM |
| Tuesday | 8:30 AM – 5:00 PM |
| Wednesday | 8:30 AM – 5:00 PM |
| Thursday | 8:30 AM – 5:00 PM |
| Friday | 8:30 AM – 3:00 PM |